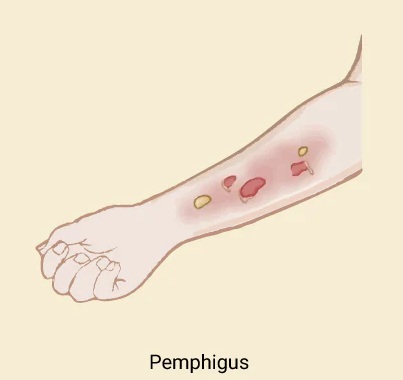
Pemphigus
In dermatology is a rare autoimmune blistering disease where the immune system attacks proteins (desmogleins) holding skin and mucous membrane cells together, causing fragile blisters that easily rupture into painful, open sores. The main types are Pemphigus Vulgaris (mouth/mucosa first, then skin) and Pemphigus Foliaceus (skin only, usually back/chest/shoulders). Diagnosis involves skin biopsy (immunofluorescence), and treatment focuses on corticosteroids and immunosuppressants to control symptoms and achieve remission.
It’s a chronic, potentially severe condition affecting quality of life due to pain, infection risk, and functional limitations.
Early diagnosis by a dermatologist is crucial for effective management, often requiring a multidisciplinary approach.
It’s important to differentiate from other blistering diseases like bullous pemphigoid, which affects deeper skin layers.
It affects people of all races, age, and sex. It most commonly appears between the ages of 30 and 60 years and is more common in Jews and Indians than in other races, presumably for genetic reasons.
Drug-induced type is also recognized and is most often caused by penicillamine, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and cephalosporins.
It is sometimes triggered by cancers particularly lymphomas and Castelman disease (paraneoplastic pemphigus), infection, or trauma.
Autoimmune Nature: The body produces autoantibodies (like IgG) that target desmogleins, disrupting cell adhesion (acantholysis).
Blister Characteristics: Unlike other conditions, blisters are flaccid and break easily, leading to erosions.
Causes of pemphigus
It is an autoimmune blistering disease. The keratinocytes are cemented together at unique sticky spots called desmosomes.
In pemphigus vulgaris, immunoglobulin type G (IgG) autoantibodies bind to a protein called desmoglein 3 (DSG3), which is found in desmosomes in the keratinocytes near the bottom of the epidermis. The result is the keratinocytes separate from each other, and are replaced by fluid (the blister). About 50% of patients also have anti-DSG1 antibodies.
Large epidemiological studies have suggested a rare link between herpes virus infection and pemphigus.
Common Types

Pemphigus Vulgaris (PV)
Most common, starts with painful mouth sores, then skin blisters (can affect genitals).
Pemphigus Foliaceus (PF)
Only affects skin (chest, back, shoulders), blisters are often itchy but don’t involve mucous membranes.
Diagnosis: A dermatologist performs a skin biopsy, often with direct immunofluorescence (DIF) to detect antibodies, and examines the blister’s depth (cell separation).

Clinical Features
Most patients with it first present with lesions on the mucous membranes such as the mouth and genitals. Blisters usually develop on the skin after a few weeks or months, although in some cases, mucosal lesions may be the only manifestation of the disease.
Skin lesions appear as thin-walled flaccid blisters filled with clear fluid that easily rupture causing itchy and painful erosions. They most often arise on the upper chest, back, scalp, and face. Erosions in the skin folds may develop into vegetative lesions which are granular and crusted (pemphigus vegetans). The skin around the nails may be painful, red, and swollen comparison to white skin, darker skin tones may differ in their presentation which can cause diagnostic delay. Diagnostic features in darker skin tones may include flaccid blister which lack erythema and hyperpigmented plaques with superficial erosion and haemorrhagic crusting. At later and more advanced stages, plaques with a pink base and surrounding hyperpigmentation are present.
The inside of the mouth is commonly involved in pemphigus vulgaris. Involvement of the pharynx and larynx cause pain on swallowing and a hoarse voice. Nasal involvement causes congestion and bleeding. The conjunctiva, esophagus, labia, vagina, cervix, penis, urethra and anus may also be affected.
Features of oral mucosal pemphigus
Oral lesions in 50–70% of patients
Superficial blistering and erosions
Widespread involvement within the mouth
Painful, slow-to-heal ulcers
Spread to the larynx causing hoarseness when talking
Difficulty eating and drinking.
Clinical Variants of pemphigus
Pemphigus vegetans
Rare subtype, characterized by vegetative plaques composed of excessive granulating tissue and crusting.
Accounts for 1-2% cases of all pemphigus and most commonly occurs at intertriginous sites, face and scalp.
Characteristic histological finding include hyperkeratosis, pseudoepitheliomatous hyperplasia and papillomatosis with acantholysis that creates a suprabasal cleft.
Two clinical subtypes
Pemphigus vegetans of Neumann (vegetative plaques arising from pemphigus vulgaris lesions)
Pemphigus vegetans of Hallopeau (plaques not preceded by bullae).
Pemphigus herpetiformis
Previously described a rare subtype of pemphigus vulgaris or pemphigus foliceus.
Characterized by urticarial plaques and vesiculobullous eruption seen in herpetiform or annular pattern.
Plaques are associated with severe pruritus and rarely involve the mucosa.
Histologically characterized by eosinophilic spongiosis, mostly without acantholysis.
Treatment options
Control blistering, minimize side effects, and achieve remission using systemic corticosteroids, steroid-sparing agents (like azathioprine), and newer therapies (like rituximab).
Complications
It can cause very extensive, life-threatening erosions, especially if the diagnosis is delayed. Other potentially severe complications
Secondary bacterial infection
Fungal infection, especially candida
Viral infection, especially herpes simplex
Nutritional deficiencies due to difficulty eating
Complications of systemic steroids especially infections and osteoporosis
Complications of immune suppressive treatments
The psychological effects of severe skin disease and its treatment (anxiety and depression)
An elevated risk of cardiovascular disease (atherosclerosis, heart failure, arrhythmia, thromboembolism and cardiovascular death).
