Perinatal mood and anxiety disorders (PMADs)
Perinatal mood and anxiety disorders (PMADs) are mental health conditions that can affect women during pregnancy and up to one year after childbirth. These disorders, which include depression, anxiety, and postpartum psychosis, can have significant consequences for maternal and infant health. PMADs are common, affecting approximately 15-20% of pregnant and postpartum women.
From the time of conception to the year after the birth of your child can be simultaneously fulfilling and extremely stressful. Motherhood brings a tremendous strain on your physical and mental health. Pregnancy demands that you are responsible and careful while you are continually concerned about the well-being of your unborn child.
Then, delivery happens ad you find that you are confronted with sleep deprivation, changing family dynamics, fluctuating hormones, and your needy baby. Certainly, this time can be filled with moments of intense bonding and joy; however, for many women depression and anxiety symptoms can surface.
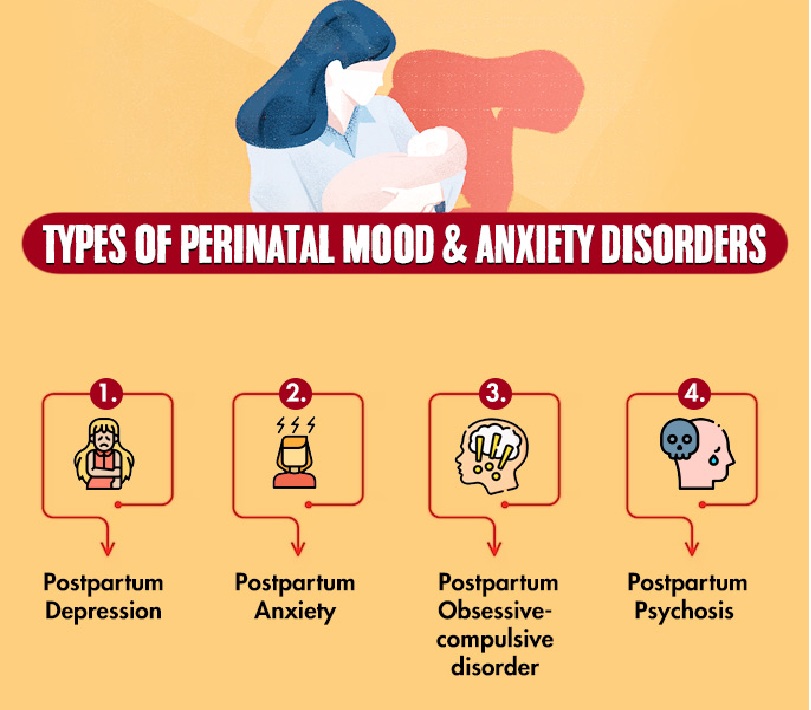
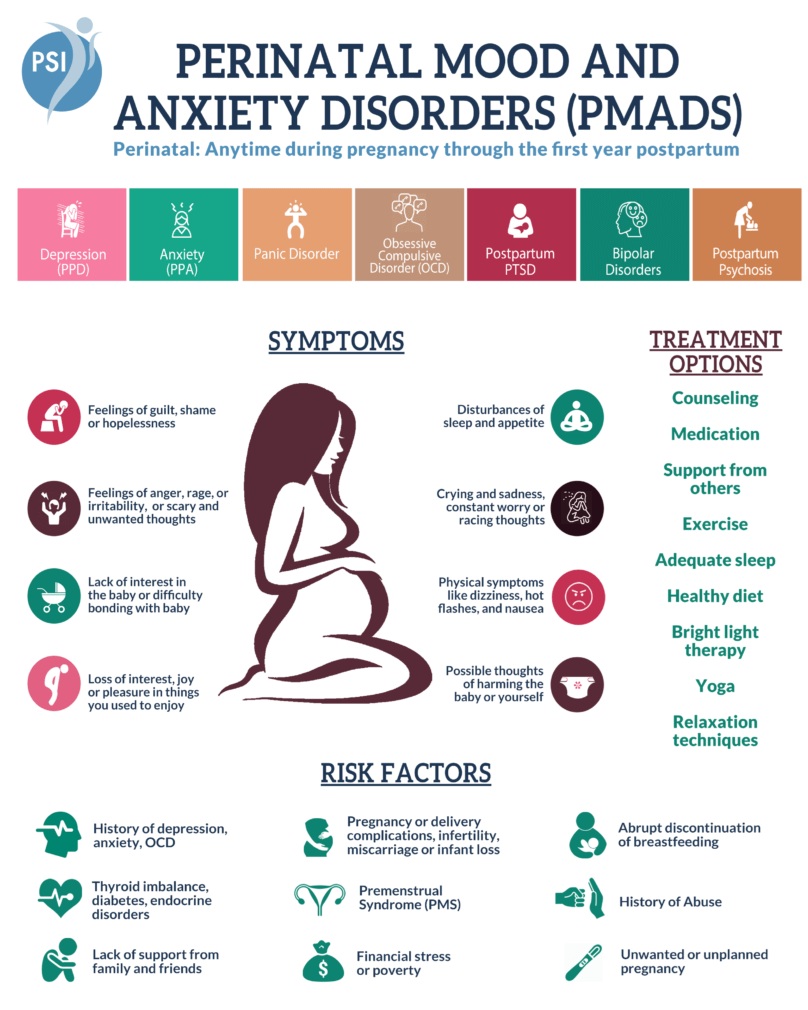
Types of Perinatal Mood and Anxiety Disorders
Depression
Feelings of sadness, loss of interest, and fatigue.
Anxiety
Excessive worry, nervousness, and fear, which can manifest physically as well as mentally.
Postpartum psychosis
A severe mental health condition that can involve delusions and hallucinations.
Obsessive-Compulsive Disorder (OCD)
Intrusive thoughts and repetitive behaviors like watching the same movies or dramas which connect with their expectations, emotions and both the positive and negative thoughts.
Post-Traumatic Stress Disorder (PTSD)
Emotional distress and symptoms following a traumatic event.
Symptoms of Perinatal Mood and Anxiety Disorders (PMADs)
Symptoms may vary, but common signs includes
Depression due to Perinatal Mood and Anxiety Disorders (PMADs)
Persistent sadness, irritability, loss of interest in activities, changes in sleep and appetite, and difficulty concentrating.
Anxiety due to Perinatal Mood and Anxiety Disorders (PMADs)
Excessive worry, restlessness, difficulty relaxing, and physical symptoms like racing heart or sweating.
Postpartum anxiety disorders such as panic disorder, obsessive compulsive disorder and generalized anxiety disorder appear to be as common as postpartum depression and even coincide with depression. Perinatal anxiety symptoms can include the following: panic attacks, hyperventilation, excessive worry, restless sleep, and repeated thoughts or images of frightening things happening to the baby.
Postpartum psychosis
Hallucinations, delusions, disorganized thinking, and changes in behavior.
Postpartum Depression (PPD)
Many women have a variety of mood symptoms in the aftermath of delivery. 50-85% of women feel Postpartum Blues or “Baby Blues” for a short time, usually 1-3 weeks after delivery. Common symptoms of “Baby Blues” can be mood instability, depressed mood, weepiness, sadness, irritability, anxiety, lack of concentration and feelings of dependency. Symptoms of “Baby Blues” usually subside 1-3 weeks after delivery. These symptoms are often self-limited and are to be distinguished from a more severe condition often called Postpartum Depression (PPD) which has increased severity and duration of symptoms.
Postpartum Depression occurs in up to 10% of births. It typically emerges over the first 2-3 months after childbirth but may occur at any point after delivery. Symptoms of PPD last for more than 2 weeks. Depression after childbirth is a serious illness and can have significant and lasting impact on the patient, infant, and family.
Risk Factors of Perinatal mood and anxiety disorders (PMADs)
History of mental health conditions.
Previous depression or anxiety.
Pregnancy complications.
Preeclampsia or other issues.
Perinatal loss.
Miscarriage, stillbirth, or infant death.
Lack of social support.
Feeling isolated or alone.
Low socioeconomic status.
Financial strain or lack of resources.
So many personality oriented different behaviors with in the child will be come out at their adolescence age.
Consequences of Perinatal Mood and Anxiety Disorders (PMADs)
Maternal health
Increased risk of poor maternal health behaviors and adverse pregnancy outcomes.
Infant health
Increased risk of preterm birth and low birth weight. Later physical and mental issues within the child.
Family relationships
Strain on relationships with partner and children.
Treatment Perinatal Mood and Anxiety Disorders (PMADs)
Therapy
Cognitive Behavioral Therapy (CBT) and other evidence-based therapies can help manage symptoms.
Medication
Antidepressants and anti-anxiety medications may be prescribed.
Support groups
Connecting with other parents experiencing similar challenges.
Medical Evaluation and Treatment
Seeking professional help from a doctor or therapist is crucial.
Screening and Early Intervention.
Screening and monitoring for physical symptoms.
Healthcare providers should screen for PMADs during prenatal and postpartum care.
Early intervention.
Early identification and treatment are crucial to prevent worsening symptoms and improve outcomes for both mother and baby.
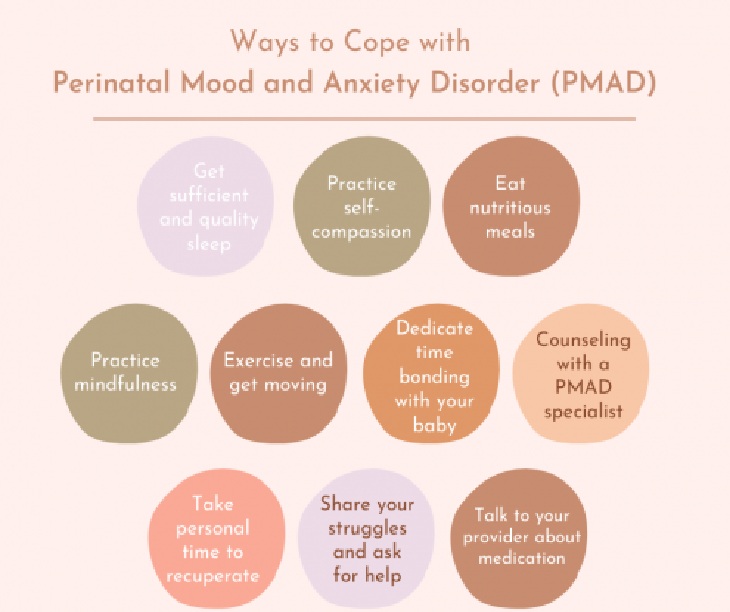
Ways to Cope with Perinatal Mood and Anxiety Disorders (PMADs)
Practice self-compassion.
Self-compassion refers to being kind and loving towards yourself, using mindfulness, and feeling a connection with others. Connect with all your innate worthiness as a human being. Notice that you are suffering and that’s okay. Practicing self-compassion soothes the autonomic nervous system and generates empathy, connectedness, and calmness. You can see PMAD as a need to seek help and reach out rather than a source of shame. Motherhood can be a time to learn, grow, and heal.
Get sufficient and deep sleep.
Although this may seem an impossible task, sleep is essential for your to recover and restore your physical and mental health. Ask your support system, such as your husband, to watch your newborn so that you can rest. You may need to take naps during the day when someone else can care for your baby. If you have the financial means, you may consider hiring a night nanny. Night nannies take care of your baby throughout the night so that you can get sleep.
Feed your body healthy foods.
A significant amount of research supports the connection between eating nutritiously and a reduction of anxiety and depression. Although fixing a nutritious meal may take some time out of your day, feeding your body nutritious foods will generate stamina and can improve your mood. Eating clean proteins, whole grains, and a large portion of diverse fruits and vegetables led to optimal cellular functioning in the gut, brain, and rest of the body. Refrain from fried, overly salty, sugary, and simple carbohydrates that may trigger inflammation and cause unhealthy fluctuations in your blood glucose levels and impair your gut microbiome.
Practice mindfulness.
Mindfulness refers to the practice of noticing your present awareness with an attitude of acceptance and non-judgment. Self-awareness allows you to be aware of your thoughts and emotions without getting “hooked” on them. You simply notice your internal experience so that you can acknowledge and accept where you’re at. With mindfulness, you are released from automatically reacting to your emotions and generate a sense of being grounded. To start, try daily meditation to develop mindfulness skills and then work up to using mindfulness throughout the day in all your activities.
Exercise and move.
Physical activity can lead to heightened mood and may reduce the intensity of PMAD symptoms. Taking a group class may offer you alone time that you need and a sense of connection with others. Alternatively, you could try walking or jogging with your baby as another way to increase physical activity. The added benefit of going outside and feeling the sun may help to improve your mood. If you are pregnant, you should contact your healthcare provider before starting any exercise routine.
Bond with your baby.
When you suffer from PMAD, you may feel disconnected from your baby. Fostering your relationship with your baby will help you to overcome these feelings. Soothing, providing reassurance, and holding your baby are just some ways to develop this bond. Playing, maintaining skin-to-skin contact, reading, singing, and talking are specific ways to create a secure attachment and empower you as a mother. When you are pregnant, you can bond with your unborn child by talking and singing, and visualizing the relationship that you will foster once he/she is born.
Remove or limit stressors.
When you are already struggling with depression and/or anxiety, any additional stressors can feel overwhelming. You may feel that you have limited capacity to take on any additional stress. You may need to say “no” and postpone certain responsibilities. Think about taking a break from time-consuming activities that are causing stress. Ask for help.
Start therapy for PMAD.
Only 40% of mothers are diagnosed with PMAD and only 60% seek treatment. Mothers should not face PMAD alone. For the health of the mother and child, engaging in psychological care is so important. Find a psychologist or counselor who specializes in PMAD treatment. In therapy, you will develop insight into what’s been bothering you, establish coping skills, learn new ways of parenting, and address any mental health issues, such as trauma.
Ask your healthcare provider for resources and treatment.
Psychiatric medication may be an option to manage your mood. Your psychiatric provider can provide you with information on the risks of medication and other treatment options.
Share your struggles.
If possible, ask your family and friends to help you through this difficult time. Share your feelings and ask for help. There is no shame in asking for help with cleaning, food preparation, or babysitting while you nap. If you are financially able, you may want to pay a babysitter to help you out on a regular basis.
When you are in a crisis, get immediate help.
If you are having thoughts about dying or harming your child, immediately reach out for help. Ensure that your baby is located in a safe place and then seek assistance.
medlight2u.com
A light on Practice of Medicine (The information provided is for informational and educational purposes only and should not be considered professional advice)
Acne Acne vulgaris Acute Renal Failure Adrenal cortex Angina Angina Pectoris Aortic Regurgitation (AR) Aortic Stenosis (AS) Chest pain Chronic pyelonephritis Coarctation of Aorta Cough cyanosis Cystic acne Dehydration depression Diabetes Mellitus Diagnosis of Aortic Stenosis Dr.KTS DR K TAMILSELVAN Fatigue Heart Failure Hypertension Hypokalemia Hypothyroidism Ischemic Heart Disease LBBB Mitral Incompetence Mitral insufficiency Mitral valve prolapse Nocturia Patent Ductus Arteriosus PDA Polyuria Proteinuria pulmonary hypertension Pulmonary Stenosis ST Depression Symptoms of Acne Syncope Treatment for acne valvular heart disease Ventricular Septal Defect VSD Zits


Leave a Reply