Kidney Transplantation
A kidney transplant is a surgical procedure that replaces a diseased or damaged kidney with a healthy kidney from a donor. It’s a treatment option for people with chronic or end-stage kidney failure.
Here are some things to know about kidney transplants.
Donor
The kidney can come from a living donor or a deceased donor. A living donor can be a family member or someone else who is a good match.
Procedure
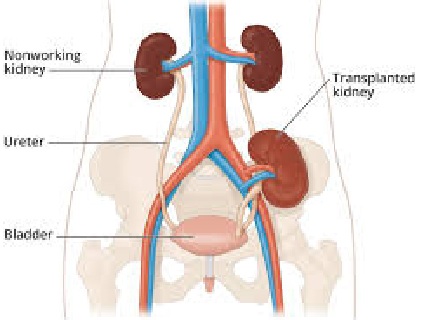
During the surgery, the surgeon places the new kidney in the lower abdomen and connects its blood vessels to the recipient’s. The diseased kidneys are usually left in place.
Recovery
It can take several weeks before you can return to your normal activities, but most people can go back to work after 6 to 8 weeks.
Medication
After the transplant, you’ll need to take drugs for the rest of your life to prevent your body from rejecting the new kidney.
Waiting list
There can be a long wait for a new kidney. Factors that may affect your wait time include your age, blood type, and where you live.
Benefits
Kidney transplants are often the preferred treatment for end-stage renal disease. Patients who have a transplant often have a better quality of life and a longer projected survival than those who remain on dialysis.
Ultimate management in End Stage Renal Disease (ESRD) is kidney transplantation
The kidney can be obtained from an HLAA (Human Leucocyte Associated Antigen) matched living related donor or from a cadaver (of a brain death individual). Proper evaluation and consent of living donor is mandatory before accepting the kidney for donation.
Absolute Contraindication
1. Reversible renal disease
2. Advanced malignancy
3. Active glomerulonephritis
4. Active peptic ulcer disease
5. Active infections
6. Ability of conservative measures to maintain life.
7. Oxalosis
8. Advanced cerebro-vascular disease of IHD.
9. Previous sensitization to donor tissue.
Relative Contraindications
1. Age should not be > 55 years)
2. Unsuitable bladder / urethra
3. Iliofemoral occlusive disease
4. Diabetes mellitus
5. Diverticulosis
6. Psychiatric problems
Donor selection and preparation
Living donor
Physical examination to exclude disease.
ABO group and HLA should be matched
Normal renal parameters
Selective renal arteriography to rule out presence of multiple or abnormal renal arteries.
Cadaveric donors
Should be free from malignant diseases
Liberal infusion with normal saline for 12 hours, preoperatively to minimize changes of acute tubular necrosis in graft kidney.
Pre transplantation Recipient Preparation
1. Dialysis at least 48 hours before transplant surgery.
2. Bowel decontamination : 48 hours prior to surgery, by oral neomycin low residue diet, and high bowel washes.
3. Immunosuppression : by following drugs.
a) Glucocorticoids (Prednisolone) 30-40 immediately prior to, or at time of, transplant surgery, continued for 2 wees, then tapered.
b) Azathioprine (Imuran) 1-2 mg / kg day immediately after transplantation and continued life long.
c) Cyclophosphamide : may substituted if hepatotoxicity or nephritis after azathioprine.
d) Cyclosporin – A. Reserved for cases of rejections or retransplant following earlier graft rejection.
e) Anti-lymphocyte globulin (ALG) and OTK3 for rejection.
Hyperacute Rejection should be suspected from
Pain, swelling and tenderness at the site of graft.
Haematuria associated with albuminuria
Significant oliguria, fever
Sudden increase in graft size assessed by radiography
Withering of cortical vessels, or beading of cortical vessels on angiography.
Renal isotope scan : showing poor uptake by renal parenchyma.
Ultrasound showing presence of perirenal collection of urine, blood or lymph.
Rise in serum creatinine level and decreases in creatinine clearance.
Final confirmation is by biopsy of graft kidney.
Treatment
Methylprednisolone 500 mg IV daily for 3-5 days.
Antithymocyte / antilymphocyte globulin
Cyclosporin + azathioprine + steroid, if no improvement, the graft is removed.
Complications following transplantation
Technical complications
i. Vascular anastomotic leak of occlusion
ii. Ureteral anastomotic leak or occlusion
iii. Ureteral rupture
iv. Lymphocele
v. Renal artery stenosis
vi. Wound infection
Immunologic : Hyperacute, acute or chronic rejection
Medical
i. Acute tubular necrosis and ARF
ii. Infections are to impaired host defense, pneumocytes carinii, Candida, Aspergillus, Cytomegalovirus, Mycobacteria
iii. Recurrence of glomerulonephritis
iv. Poor wound healing
v. steroid-psychosis
vi. Gastro-intestinal bleeding
vii. Leucopenia, thrombocytopenia
viii. Hypercalcemia
ix. Myocardial infarction & stroke
x. Aseptic necrosis of femur
Prognosis
One year graft survival in HLAA matched living related homograft approaches 94% using blood transfusion protocol from haplotype matches, living related donor; one year graft survival approaches 90% with matching of the HLAA and use of multiple nonspecific blood transplantation; one year graft survival of cadaver renal transplant are at risk of dying each year. The risk of death increases if the has diabetes or systemic disease.
Renal Failure with Hemoptysis
Good pastures syndrome
Wegener’s granulomatosis
Henoch-Schonlein purpura
PAN, SLE, cryoglobulinemia
Renal vein thrombosis with pulmonary embolism
Acute renal failure with pulmonary oedema
Right-sided infective endocarditis with septic pulmonary emboli and immune-complex nephritis.
Infection-tuberculosis, legionnaires disease.
Renal Disease with Jaundice
Haemolytic-uraemic syndrome
Hepatorenal failure (hepatic nephropathy)
Leptospirosis (Weil’s disease)
Hepatitis B with nephritic syndrome
Alcoholic cirrhosis with IgA nephropathy or renal tubular acidosis.
Polycystic disease with congenital hepatic fibrosis
Staffers syndrome : renal cell carcinoma with non-metastatic hepatic dysfunction (e.g. cholestasis)
Toxic : methoxyflurane
Renal disease with small kidneys
Chronic glomerulonephritis (symmetrically smooth)
Chronic pyelonephritis (asymmetrically scarred)
Post-obstructive atrophy
Renovascular insufficiency
Late stage of many disease causing large kidneys initially
Renal Disease with large kidneys
Acute glomerulonephritis
Acute interstitial nephritis
Acute tubular (or cortical) necrosis
Acute urate nephropathy
Polycystic disease
Medullary sponge kidneys
Obstructive uropathy (hydronephrosis)
Early stage
Amyloidosis (+ myeloma)
Renal vein thrombosis
Insulin – dependent diabetes
Malignancy (leukemia / lymphoma, Wilms’s tumor, Gradwitz tumor)
Miscellaneous : Acromegaly, hepatic cirrhosis, hemophilia, sickle-cell anaemia, vasculitis, radiation nephritis.
Compensatory hypertrophy
Nocturia : Diagnosis Significance
Prostatism
Edematous states
Salt-losing nephropathies, e.g.
Analgesic nephropathy
Medullary sponge kidneys
Sickle cell disease
Polyureic states e.g.
Diabetes mellitus; insipidus
Primary Polydipsia
Post – ATN
Bladder pathology
Tumor, fibrosis, infection
Loss or reflux inhibition e.g. multiple sclerosis
Vesico-ureteric (double micturition in children)
Causes of papillary necrosis
Analgesic abuse, esp., phenacetin
Obstructive uropathy, esp., with infection
Acute pyelonephritis, esp., in diabetes mellitus
Sickle cell disease
Renal tuberculosis
Dysproteinemia
Causes of Sterile Pyuria
Renal tuberculosis
Analgesic nephropathy
Renal calculi, polycystic disease
Urinary infection treated with chemotherapy
Nephrotoxic drugs
Nonspecific urethritis
Chronic prostatitis, interstitial cystitis, herpetic urethritis
Differential diagnosis of Normoglycemic Hypercalciuria
Idiopathic
Medullary sponge kidneys
Immobilization (esp.in Paget’s disease)
Sarcoidosis
Acromegaly, Cushing’s syndrome
(Mild) primary hyperparathyroidism (may be definitively diagnosed by documenting elevated serum pTH and / or Urinary Cyclic Adenosine Mono-Phosphate (cAMP)
Renal tubular acidosis
Iatrogenic : Corticosteroids, frusemide
Disproportionate Elevation of Blood Urea and Creatinine
Dehydration (loss of water and sodium)
Gastrointestinal haemorrhage
Congestive cardiac failure
High protein intake
Drugs : Tetracycline, Corticosteroids
Cyclosporin A
Pathological Spectrum of Renal Tubular Dysfunction
(X = X-linked, A = autosomal, R = recessive , D = dominant )
1.Defective tubular responsiveness to hormones
Nephrogenic diabetes insipidus (XR : distal tubular dysfunction)
Batters syndrome (A,R Distal)
Ladles syndrome (AD, distal)
Pseudohyponatremia rickets (XD, proximal)
2.Primary tubular transport defects (often associated with corresponding intestinal transport defects)
Renal glycosuria (AD, proximal)
Hartnup disease (AR proximal)
Cystinuria (AR, proximal)
Cystinosis (AR, proximal : leads to uremia and death in childhood)
Fanconi syndrome (AR, proximal, multiple defects)
Renal tubular acidosis type 1 (AD distal)
3. Secondary tubular transport defects
a) Distal tubule defects : in liver disease, Medullary sponge kidneys, infantile polycystic disease, Amphotericin B, Cyclosporin A toxicity, Lithium
b) Proximal tubule defects : in Wilson’s disease, heavy metal poisoning, medullary cystic disease
c) Distal and / or proximal defects in Myeloma, Sjogren’s syndrome, other auto-immune disorders. Renal transplant rejection, Long-standing hypercalciuria / anemia hypokalemia, Obstructive uropathy, Analgesic nephropathy, chronic pyelonephritis.
When to suspect Renal Tubular Acidosis
High urine pH > 6 despite acidemia (in distal RTA) and negative urine culture.
Hyperchloremic hypokalemic acidosis
Normal anion gap
Hypouricemia and hypophosphatemia (proximal TA)
Hypercalciuria : low urinary specific gravity : polyuria : failure of urinary acidification following oral ammonium chloride 100 mg / kg (distal RTA)
Hyperkalemia and acid urine : Hyporeninemic hypoaldosteronism in elderly diabetics or obstructive uropathy (RTA Type 4)
Spectrum of Renal Pathology in Diabetes
Renal enlargement (in early insulin – dependent diabetes ) osmotic polyuria
Diffuse glomerulosclerosis
Nodular glomerulosclerosis (kimmelstiel Wilson disease – Wilson lesions) : suggests insulin-dependent diabetes
Glycogen deposition in tubules (Armanni-Ebtein lesion)
Interstitial nephritis
Pyelonephritis – papillary necrosis
Recurrent urinary tract infections
Hyporeninemic hypoaldosteronism.
medlight2u.com
- Oral cancer
- Gestational Trophoblastic Neoplasia (GTN)
- Brain tumors
- Perinatal Mood and Anxiety Disorders (PMADs)
- Unstable mind
Great content! Super high-quality! Keep it up!
I’m so in love with this. You did a great job!!
new texts were rewritten
The articles you write help me a lot and I like the topic
Acne Acne vulgaris Acute Renal Failure Adrenal cortex Angina Angina Pectoris Aortic Regurgitation (AR) Aortic Stenosis (AS) Chest pain Chronic pyelonephritis Coarctation of Aorta Cough cyanosis Cystic acne Dehydration depression Diabetes Mellitus Diagnosis of Aortic Stenosis Dr.KTS DR K TAMILSELVAN Fatigue Heart Failure Hypertension Hypokalemia Hypothyroidism Ischemic Heart Disease LBBB Mitral Incompetence Mitral insufficiency Mitral valve prolapse Nocturia Patent Ductus Arteriosus PDA Polyuria Proteinuria pulmonary hypertension Pulmonary Stenosis ST Depression Symptoms of Acne Syncope Treatment for acne valvular heart disease Ventricular Septal Defect VSD Zits



Can you write more about it? Your articles are always helpful to me. Thank you!