Intestinal Tuberculosis
Intestinal tuberculosis (ITB) is a rare infection of the digestive tract caused by the Mycobacterium tuberculosis organism. It’s a type of gastrointestinal (GI) tuberculosis (TB).
Gastrointestinal tuberculosis is caused by Mycobacterium tuberculosis infection, usually after coming in contact with the respiratory fluids of a person who got already infected. This bacterium can travel from lungs to Gastro-Intestinal tract through your blood and lymph systems or via your swallowing infected phlegm.
Less commonly, gastrointestinal tuberculosis can develop from the ingestion of milk products infected with Mycobacterium bovis a similar bacterium that can affect cows.
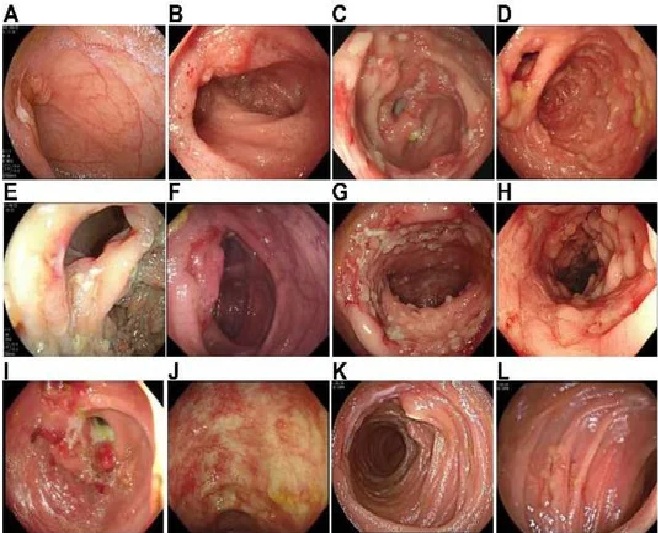
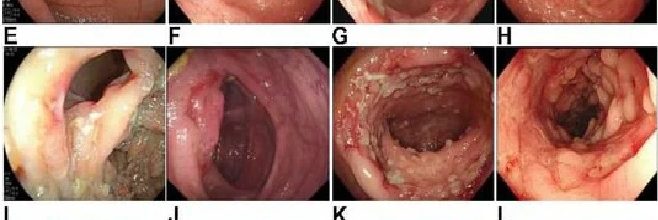
(A) Ulcer in the terminal ileal; (B) inflammation and erosion in the terminal ileal; (C) ulcer in the ileocecal region; (D) inflammation and erosion in the ileocecal region; (E) ileocecal valve deformation; (F) inflammation and erosion in the ileocecal valve; (G) pseudo polyps and colonic ulcer; (H) colonic inflammation; (I) colonic stricture and colonic mass; (J) colonic scar; (K) jejunal ulcer; and (L) small intestinal inflammation.
Gastrointestinal tuberculosis can affect various parts of your GI tract
Esophagus, in rare cases
Stomach
Small intestines
Large intestines
Rectum and anus
Intestinal Tuberculosis commonly involve caecum, mesenteric lymph nodes and peritoneum. Mostly human strain is responsible, usually dissemination from lung lesion. Intestinal lesion may be ulcerative or hypertrophic, where as peritoneal lesion is ascetic or plastic.
Extrapulmonary tuberculosis
Tuberculosis that occurs outside your lungs is called extrapulmonary tuberculosis.
It makes up about 15–20% of cases of tuberculosis infection.
The most common places extrapulmonary tuberculosis develops
Lymph nodes: 50%
Lungs: 19%
Genitals or urinary system: 13%
Bones and joints: 6%
GI system: 6%
Central nervous system: 3%
Causes of Intestinal Tuberculosis
Swallowing infected sputum
Ingesting milk from cows with bovine TB
Ingesting infected animal products.
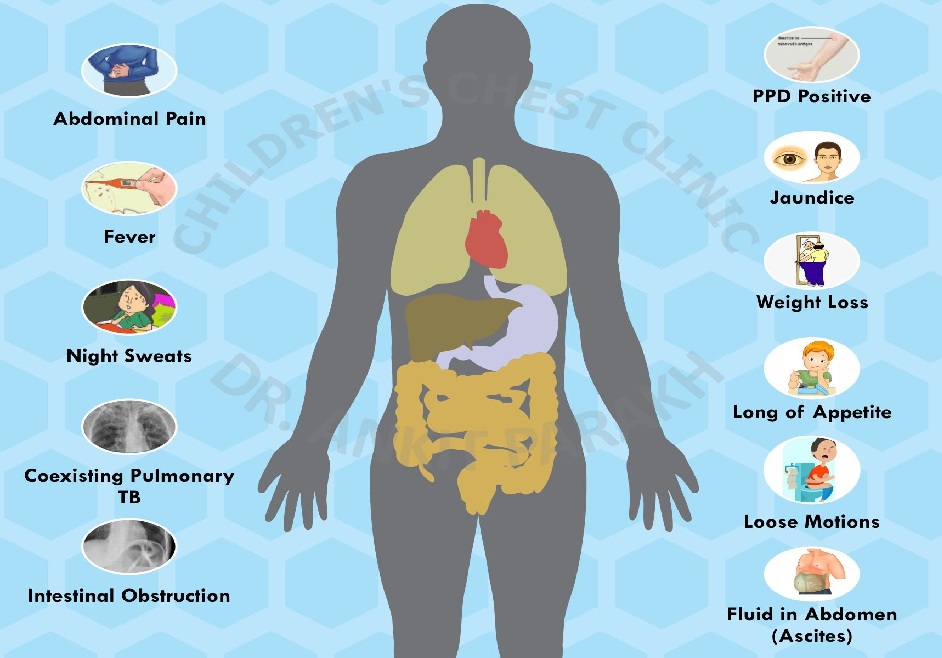
Symptoms of Intestinal Tuberculosis
Gastrointestinal tuberculosis can cause symptoms that mimic those of many other GI conditions like Crohn’s disease or cancer.
The most common part of the GI tract affected is the end of your small intestines. In a 2023 autopsy study, 96% of more than 4,500 people with gastrointestinal tuberculosis had involvement in this area, with 10% also having involvement in the first part of the large intestines called the cecum.
Abdominal pain
Intestinal swelling
Intestinal obstruction
Hematochezia
Palpable abdominal mass
Fever
Weight loss
Night sweats
Changes in bowel habits, such as diarrhea
Clinical presentation of Intestinal Tuberculosis
Abdominal pain, diarrhea, malabsorption syndrome, weight loss, low grade fever.
Subacute recurrent intestinal obstruction.
Ascites, hepatosplenomegaly.
Diagnosis of Intestinal Tuberculosis
Early diagnosis and treatment can significantly improve the outlook.
A combination of radiologic, endoscopic, microbiologic, histologic, and molecular techniques
Colonoscopy to look for ulcers, nodules, and other abnormalities.
The gold standard test for gastrointestinal tuberculosis is a bacterial culture created using a tissue sample from your intestinal mucosa collected with a long, thin tube called an endoscope.
Other tests for gastrointestinal tuberculosis include:
Imaging tests like X-rays or ultrasound
Colonoscopy
Blood Investigation
high C-reactive protein
low hemoglobin
low serum albumin
Doughy abdomen, palpable mass in ileocecal region.
Loculated ascites.
Thick narrow irregular caecum drawn upwards in barium meal follow through and evidence of intestinal obstruction.
Exudative ascites, negative on ordinary culture.
Tubercular nodules on peritoneum in Peritoneoscopy and adhesion of bowel loops.
Lack of barium retention in involved segment or persistent narrow stream of barium in involved segment (string sign)
Filling defect in caecum in hyperplastic tuberculosis.
Broad based triangular appearance of terminal ileum with base towards caecum ( Fleischer sign )
Primary hypertrophic cecal tuberculosis can mimic colonic malignancy.
Treatment for Intestinal Tuberculosis
Medication
Anti-tuberculous drugs and Surgery in cases that develop complications.
High protein, low fat and low fiber diet with enzymes and vitamins
Localized resection if there in bowel obstruction, tuberculous ulcer perforation or localized hyperplastic lesion.
Without treatment, Intestinal Tuberculosis can lead to death in 6–20% of cases.
Complications of intestinal tuberculosis
Potential complications of gastrointestinal tuberculosis
Bleeding in your GI tract
Fistulas, where part of your GI tract becomes connected somewhere it shouldn’t bowel obstruction
Stricture
Intussusception
Perforation
Anemia
Malnutrition or malabsorption
Weight loss
Vitamin and mineral deficiencies
Risk factors of Intestinal Tuberculosis
Being in close contact with people who have TB.
Immigrants to the other countries.
Immigrating from parts of the world with high rates of tuberculosis.
The homeless, Prisoners, Residents of long-term care facilities, and the immunocompromised.
Working or spending time in
hospitals
homeless shelters
prisons
nursing homes
residential homes for people with HIV
smoking
heavy alcohol consumption
illicit drug use
Conditions that weaken your immune system
HIV
Severe kidney disease
Crohn’s disease
Head and neck cancer
Receiving an organ transplant.
medlight2u.com
A light on Practice of Medicine (The information provided is for informational and educational purposes only and should not be considered professional advice)
Acne Acne vulgaris Acute Renal Failure Adrenal cortex Angina Angina Pectoris Aortic Regurgitation (AR) Aortic Stenosis (AS) Chest pain Chronic pyelonephritis Coarctation of Aorta Cough cyanosis Cystic acne Dehydration depression Diabetes Mellitus Diagnosis of Aortic Stenosis Dr.KTS DR K TAMILSELVAN Fatigue Heart Failure Hypertension Hypokalemia Hypothyroidism Ischemic Heart Disease LBBB Mitral Incompetence Mitral insufficiency Mitral valve prolapse Nocturia Patent Ductus Arteriosus PDA Polyuria Proteinuria pulmonary hypertension Pulmonary Stenosis ST Depression Symptoms of Acne Syncope Treatment for acne valvular heart disease Ventricular Septal Defect VSD Zits

Leave a Reply