Pneumonia
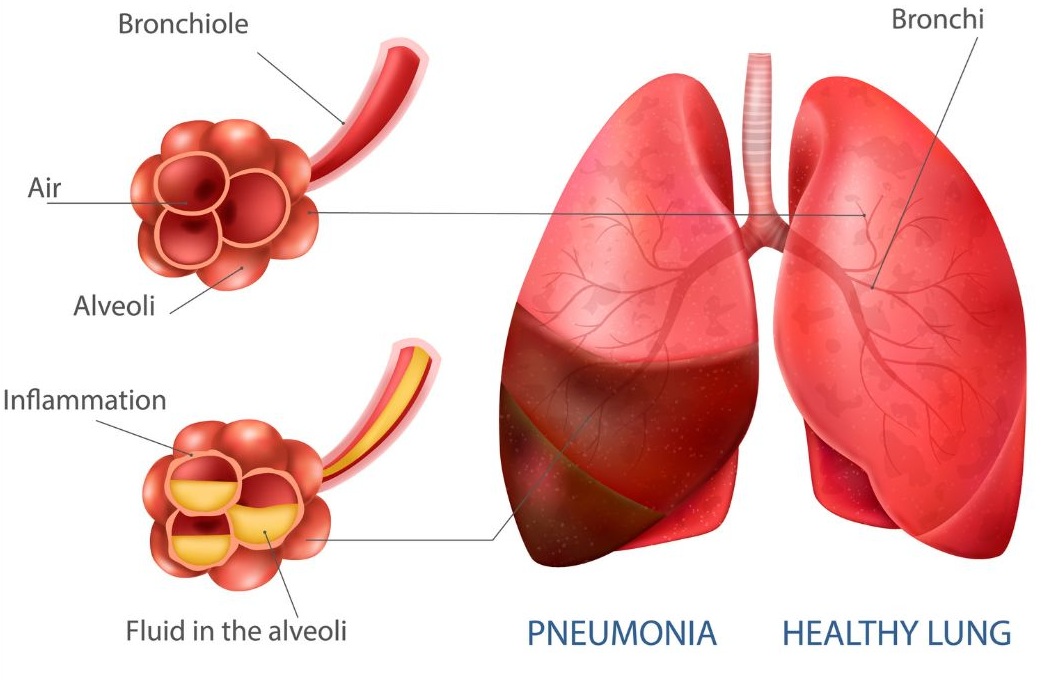
It is a condition which denotes inflammation of the lung parenchyma. Pneumonia is a serious lung infection that causes the air sacs in the lungs to fill with fluid or pus
An acute inflammation of the lungs, usually caused by inhaled pneumococci of the species diplococcus pneumonia. The alveoli and bronchioles of the lungs become plugged with a fibrosis exudates.
Anatomical Classification of Pneumonia
Lobar Pneumonia
Due to virulent organisms such as pneumococci (Type-3), Friedlander’s (klebsiella), Staph aureus. Segmental: Due to organisms of low virulence.
Certain types of pneumococci.
Streptococci, H. influenzae, Vincent’s spirochetes, fusiform bacilli.
Lobular Pneumonia (Bronchopneumonia if bilateral)
Occurs in elderly patients and babies, debilitated patients. Organisms are: H. influenzae, pneumococci, streptococci, tuberculosis.

Etiological Classification
1. Infective
i. Bacterial: Pneumococcal, Klebsiella (Friedlander’s), Influenzas, Neisseria meningitis, Mycobacterium tuberculosis, Brucella, Salmonella, Staph aureus, Legionella pneumophila
ii. Viruses and small bacteria: Influenzae and para influenzae, measles and chickenpox, adenoviruses, respiratory syncytial ‘ viruses, chlamydia, Mycoplasma, pneumoniae.
iii. Rickettsia: Coxiella burnet (Q fever), Typhus,
iv. Yeasts and fungi: Actinomycosis, Candida, histoplasmosis, aspergillus, Cryptococcus neoformans.
v. Protozoa and parasites: Pneumocystis carinii, amoebae, toxoplasma.
2. Allergic
(i) Collagen vascular disease (PAN),
(ii) Steven Johnson syndrome.
3.Chemical Agents
(i) Irritant gases: Ammonia, Sulphur dioxide, chlorine,
(ii) Irritant liquids: Lipoid pneumonia.
4. Physical Agents
Irradiation.
Clinical classification of Pneumonia
Community Acquired Pneumonia (CAP)
Nosocomial (Hospital acquired)
In immunosuppressed patients
Causes of Pneumonia
Pneumonia can be caused by bacteria, viruses, or fungi
Primary: 4 Is
Infection
Bacterial: Pneumococcus, staphylo, etc.
Influenza (Viral), respiratory syncytial
Rickettsia: Q fever
Mycoplasma: M. pneumoniae
Yeast and fungi: Candida, actino, histoplasma.
Protozoa and parasites : Toxoplasma, amoeba.
Immunological
Polyarteritis.
Irritation
Gas: Chlorine, ammonia, SO2
Liquids: Vomit, lipid pneumonia Irradiation.
Secondary : In association with
Aspiration from nasopharynx
Bronchiectasis
Carcinoma of lung
Depression of defenses (3S)
Systemic disease
Steroids
Suppressive (immune) drugs
Symptoms of Pneumonia
Symptoms can range from mild to severe
Cough with or without mucus
Fever
Chills
Trouble breathing
Sharp pain in your chest or belly when you breathe or cough
Fatigue
Loss of appetite
Nausea, vomiting, or diarrhea
A bluish tint to your lips or fingernails
Special features of Pneumonia
Pneumococcal : Lobar consolidation. Can result in most severe pneumonia. Good resolution.
Staphylococci : Abscess formation.
Human influenza : Principally in patients with underlying chest disorder (e.g. COPD).
Legionella spp. : Important cause of CAP and nosocomial pneumonia.
Often severe illness.
Klebsiella : Blood tinged sputum. Patchy consolidation.
Tuberculous : Usually apical No response to antibiotics.
Viral : More symptoms than signs.
Failure to improve on therapy
Antibiotic resistance
Bronchial obstruction, bronchiectasis
Complications: Abscess, empyema
Diagnostic error example pulmonary embolism, bronchial Carcinoma, fibrosing alveolitis
Endocarditis and other metastatic complications.
Faulty (inadequate) dosage
General factors
Hypoxia, dehydration,
Immunocompromised patient
Recurrent pneumonia
1. Respiratory disease
Bronchial obstruction
Intraluminal: Foreign body
Intramural: Growth, stenosis
Extramural: Compression by lymph nodes
Local bronchopulmonary disease
Localized bronchiectasis
Carnified lung due to chronic pneumonia
Generalized Bronchiectasis, cystic fibrosis, chronic bronchitis
2. Non-respiratory disease
Recurrent aspiration : Alcoholics, epileptics
Immune deficiency states
Predisposing Factors of Pneumonia
Altered consciousness due to alcoholism, cranial trauma, seizures, General anesthesia, drug overdose, cerebrovascular disease.
Old age: Depresses cough and glottic reflexes.
Pain from trauma.
Thoracic/upper abdomen surgery. Impede effective coughing and lead to aspiration.
Neuro muscular disease.
Weakness from malnutrition.
Kyphoscoliosis.
Severe obstructive lung disease.
Endotracheal tube/tracheostomy.
Impairment of muco-ciliary transport – Smoking, alcohol, old age, viral infection.
Acquired immunodeficiency syndrome (AIDS)
Impairment of alveolar macrophage function due to: smoking, starvation, anaemia, pulmonary edema, viral respiratory infection also predispose to pneumonia.
Types of pneumonia
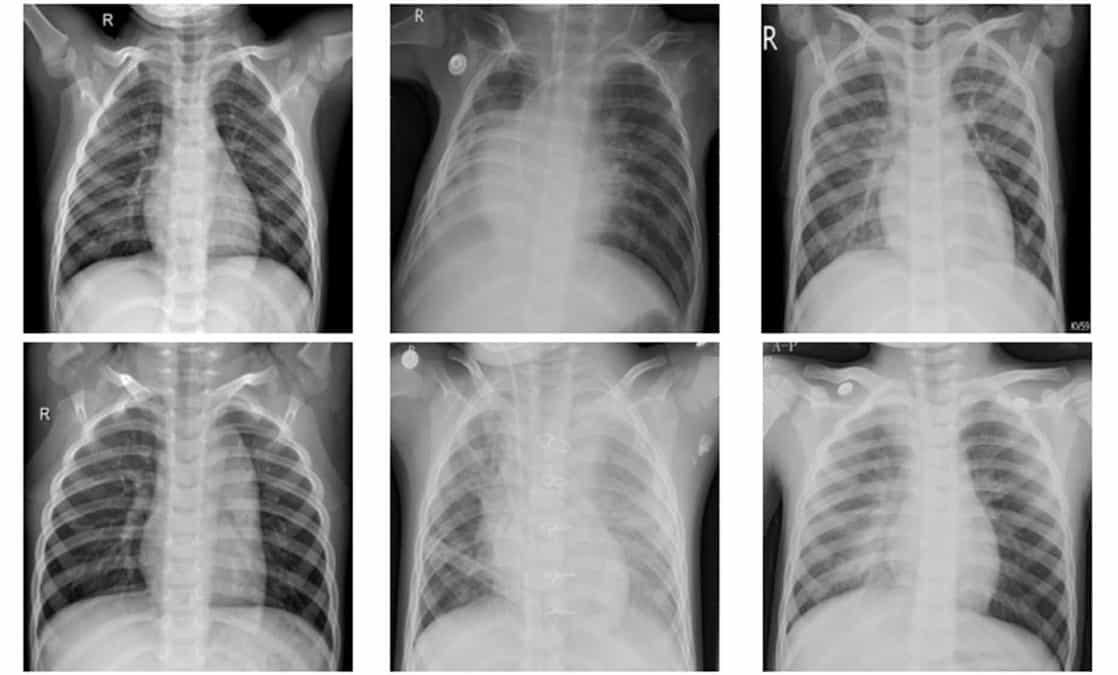
Airspace pneumonia – example : pneumococcal pneumonia.
Nonsegmental consolidation with positive air bronchogram.
Interstitial pneumonia example : mycoplasma and viral pneumonia; inflammation only involves interstation, hence reticular appearance
Bronchopneumonia: – Inflammation of terminal and respiratory bronchioles. Hence segmental infiltration without air bronchogram.
Clinical Features of Pneumonia
Fever, Tachypnoea, Pleuritic pain.
Cough with expectoration (rusty in pneumococcal pneumonia).
Signs of consolidation i.e., dull percussion note, increased VF and VR, bronchial breathing.
Investigations of Pneumonia
Sputum Gram stain and culture.
Serology for mycoplasma, chlamydia, legionella, viruses.
Chest X-ray: may show consolidation and parapneumonic effusion.
CT scan if X-ray is equivocal.
Complication of Pneumonia
1. Pulmonary
Delayed resolution, bronchiectasis, lung abscess.
2. Pleural
Pleural effusion, Empyema, Pyopneumothorax.
3. Cardiovascular
Endocarditis, pericarditis, pericardial effusion, peripheral circulatory failure.
4. Neurological
Meningism, pneumococcal meningitis, cerebral abscess.
5. Nonspecific
Herpes labialis, septicemia (and shock) cardiac arrhythmias, cardiac failure, deep vein thrombosis.
Risk factors of Pneumonia
People at higher risk of developing pneumonia include:
Infants and young children
Adults 65 or older
People who have other health problems
Staphylococcal Pneumonia
Patchy bronchopneumonia progressing over few hours to Pleural effusion and Pyopneumothorax.
Extensive, often bilateral involvement.
Multiple, thin walled cavities widely distributed.
Klebsiella Pneumonia
Occurs in debilitated immunosuppressed or diabetic children.
Patients may often have existing lung abscess or bronchiectasis.
Can involve upper lobes, also may be bilateral.
X-ray shows dense infiltrates with bulging fissures.
Currant jelly sputum in older children.
Toxic looks disproportionate to fever.
Empyema is quite common.
Mycoplasma pneumonia
Gradual onset of symptoms; intense headache
Cough is a prominent finding and sore throat is constant; scanty sputum.
Symptoms are more severe in comparison to scanty physical signs.
Normal total leukocyte and differential leukocyte count.
Patchy infiltration in the lungs but no pleural reaction.
Hemolysis use to cold hemagglutinin (IgM) may occur.
Treatment is with tetracycline or erythromycin 500 mg qid for 10 days.
Legionella pneumonia
Bilateral patchy infiltration
Toxic look, hemoptysis
Confusion, high fever
Treated with erythromycin 500 mg qid along with rifampicin 600 mg.
Pneumocystis pneumonia
Fever, dry cough, tachypnea
Ground glass opacity of lung (interstitial pneumonia)
Often bilateral, paucity of signs
Treatment with TMP-SMX
Viral pneumonia
Minimum symptoms, ache and pain
Bilateral involvement, florid signs
Influenza virus mostly the causative agent.
Acyclovir 200 mg 5 times daily x 5 days for influenza, and vidarabine 10 mg/kg x 5 day for varicella pneumonia.
Chemotherapy of Pneumonia
It is usually given by antibacterial drugs for fourteen days. Radiological clearance takes about 4 weeks.
Antibiotic regimen: Ampicillin 500 mg 6 hourly, Amoxycillin 500 mg tid, Cephalosporin 500 mg 6 hourly, cefadroxil 50 mg bid, Ciprofloxacin 500 mg bid, IV cefoperazone, IV cefotaxime l gm bid, Inj. cloxacillin 500 mg 6 hourly for S aureus
Jaundice in pneumonia
Hemolysis in mycoplasma pneumonia
Lung cancer with hepatic metastasis
Septicemia
Legionella infection
Drug induced
Hepatitis in pneumococcal infection.
Causes of Delayed Resolution
Pleural infection.
Tuberculosis.
Malignancy (bronchial obstruction by tumor).
HIV disease, immunocompromised.
Pneumonia, diagnosis and treatment
| Organism | Sputum and x – ray | Treatment |
| Pneumococcal | Gm +ve diplococci Lobar consolidation | Penicillin G or Amoxycillin |
| H. influenzas | Pleomorphic gm-ve cocobacilliLobar consolidation | Cefotaxime of ceftriaxone |
| Staph aureus | Gm +ve cocci in clumps Patchy infiltrate | Cloxacillin or vancomycin |
| Klebsiella Pneumonia | Gm -ve encapsulated rods, lobar consolidation | Cefotaxime or ceftriaxone plus aminoglycoside |
| Pseudomonas aeruginosa | Gm-ve rods patchy infiltrate and cavitation | Carbenicillin + aminoglycoside |
| Anaerobes | Mixed flora patch infiltrate | Clindamycin or penicillin +metronidazole |
| Mycoplasmapneumonae | No bacteria, increased PMN Extensive infiltration | Erythromycin or doxycycline |
| Legionella Pneumophilla | No bacteria patchy consolidation | Macrolide with rifampin |
| Chlamydia Pneumonia | Nonspecific SubsegmentalInfiltrate | Doxycycline or erythromycin |
| Moraxellacatarhalis | Gm-ve diplococci usually patchy but can be lobar | MP-SMX or cefuroxime / cefotaxime |
| Pneumocystis carinii | Non specific diffuse interstitial and alveolar infiltrate | TMP-SMX or pentamidine plus prednisolone |
The Eosinophilic Pneumonias
1.Etiology known
a. Allergic bronchopulmonary aspergillosis
b. Parasitic infestations :-microfilaria.
c. Drug reactions
2.Idiopathic
a. Loeffler’s syndrome
b. Chronic eosinophilic pneumonia
c. Allergic granulomatosis of Churg and Strauss
d. Hypereosinophilic syndrome.
Recurrent pneumonia at same site
Foreign body
Bronchial obstruction by neoplasm – benign/malignant
Bronchiectasis
Lung sequestration
Bad prognosis in pneumonia
Old age
Hypotension, tachypnoea
Very high leukocytosis/leucopenia
Hypoxemia
Extensive involvement.
Hypersensitivity Pneumonitis
|
Disease |
Causative agent |
| Farmer lung | Thermophilic actinomycetes |
| Bird fancier’s | Parakeet, pigeon, dove, |
| breeders, or handler’s lung | chicken, turkey protein |
| Humidifier or | Thermophilic actinomycetes, |
| air-conditioner lung | Aureobasidium pulluans, |
| Woodworker’s lung | Wood dust; Alternaria |
| Sauna taker’s lung | A. pullutans |
| Bagassosis | Thermophilic actinomycetes |
| Malt workers’ lung | Aspergillus fumigatus, A clavatus |
| Mushroom worker’s lung | Thermophilic actionmycetes |
| Sequoias | Aureobasidium graphium species |
| Maple bark stripper’s disease | Cryptostroma corticated |
| Coffee worker’s lung | Coffee bean dust |
| Miller’s lung | Infested wheat flour |
| Bathtub refinisher’s lung | Toluene diisocyanate (TDI) |
| Chemical workers’ lung | Toluene diisocyanate (TDI),methylene diisocyanate (MDI)phthalic anhydride, vinyl chloride |
Clinical features, diagnosis
Sudden chill, fever, cough, dyspnea on exposure to offending agent.
Bilateral basal crepitations but no rhonchi.
X-ray: nodular opacities sparing apices of lungs.
Restrictive pattern in PFT and 4-diffusion capacity.
AB G shows hypoxemia.
Antibody against precipitating agent in serum.
Treatment of Pneumonia
Treatment depends on the type and severity of the pneumonia
Bacterial pneumonia is usually treated with antibiotics.
Viral pneumonia a doctor may prescribe antiviral medications if influenza is the cause.
Fungal pneumonia is usually treated with antifungal medications
Subacute hypersensitivity pneumonitis occurs in 15% that gradually progress to lung fibrosis and respiratory insufficiency.
medlight2u.com
A light on Practice of Medicine (The information provided is for informational and educational purposes only and should not be considered professional advice)

Leave a Reply