Upper Gastrointestinal Bleeding

Upper-Gastro-intestinal bleeding is manifested as hematemesis (blood vomiting) and Malena (black tarry stool). Hematemesis usually indicates bleeding proximal to the ligament of Treitz and malena usually denotes bleeding from the esophagus, stomach or duodenum, but lesions in jejunum, ileum and even ascending colon may cause Malena provided that there is stasis. 60ml of blood is required to produce a single black stool.
Common causes for Upper GI Bleeding
Peptic ulceration, erosive gastritis, Mallory Weiss syndrome, esophageal varices, esophagitis, carcinoma esophagus and stomach, vascular ectasia, Osler-Weber-Rendu disease (Hereditary hemorrhagic telangiectasia), bleeding diathesis etc., Dieulafoy’s lesion (It is a medical condition characterized by a large tortuous artery most commonly in the stomach wall (submucosal) that erodes and bleeds. Aberrant gastric submucosal artery)
Diagnosis and Evaluation for Upper GI Bleeding
A. History and physical examination to ascertain cause
B. Assessment of blood loss
Evidence of shock (hypotension, tachycardia, sweating, metabolic acidosis). Suggest severe blood loss.
Postural hypotension (fall of BP>10mm Hg & rise in pulse rate > 20/min) when present indicate > 20% loss of blood volume.
Oliguria (urine out put <20-30ml/hr. in absence of renal disease) when present massive bleed.
Gastric aspiration by nasogastric tube may show significant fresh blood.
Investigations for Upper GI Bleeding
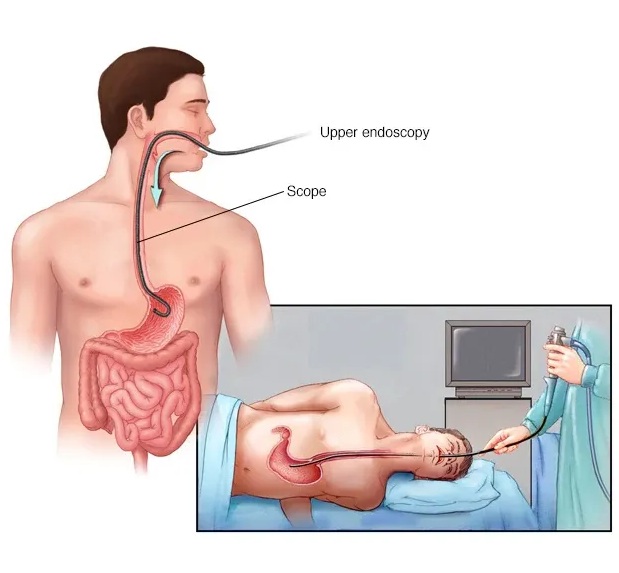
(1) Endoscopy to identify site of bleeding or visible vessel,
(2) Barium meal X-Ray identifies potential source of bleeding but fails to identify erosive gastritis or Mallory-Weiss syndrome,
(3) Arteriography selective abdominal angiography may localize site of bleeding when rate of bleeding more than 0.5ml / min.
Treatment for Upper GI Bleeding
A. General Treatment
Gastric lavage with ice cold saline
Blood transfusion if pulse rate>100/m or systolic
B.P. < 100mm.Hg.
CVP monitoring
B. Specific treatment
1. Peptic ulcer bleeding is controlled by H2 receptor antagonists.
Laser photocoagulation : Argon and NDYAG lasers are the most common endoscopic therapeutic measure used for peptic ulcer bleeding in advanced centers.
Endoscopic hemostasis by spraying over the bleeding points through the endoscopy using following agents: acrylic polymers thrombin cryoprecipitate, iron-oil mixture with an external electromagnet.
Endoscopic injection sclerotherapy injecting sclerosing agents in and around the bleeding site has proved a successful therapy recently (80-100% success rate). Heater probe application is another alternative.
Intra arterial embolization of bleeding vessel
Emergency surgery if continued or recurrent bleeding.
Elective surgery in those with chronic ulcer which have bled or requiring corticosteroid / aspirin therapy or whose supervision is difficult.
2. Variceal bleeding is controlled by
Balloon tamponade (by Sang taken-Black more tube) has shown good efficacy rate. The balloons (Esophageal, gastric) are kept inflated for 24 hours, complications include ischemic necrosis, perforation esophagus, asphyxia.
Endoscopic sclerotherapy is now a successful method of obliterating the varices and controlling upper G.I. bleeding sclerosing agents.
Endoscopic banding of varices is very easy and effective surgery; ligation of varices, esophageal transaction, shunt operation to reduce portal hypertension. (TIPSS).
Prognosis of Upper GI Bleeding
Mortality still remains around 30% in spite of advanced therapy.
medlight2u.com
A light on Practice of Medicine (The information provided is for informational and educational purposes only and should not be considered professional advice)
Acne Acne vulgaris Acute Renal Failure Adrenal cortex Angina Angina Pectoris Aortic Regurgitation (AR) Aortic Stenosis (AS) Chest pain Chronic pyelonephritis Coarctation of Aorta Cough cyanosis Cystic acne Dehydration depression Diabetes Mellitus Diagnosis of Aortic Stenosis Dr.KTS DR K TAMILSELVAN Fatigue Heart Failure Hypertension Hypokalemia Hypothyroidism Ischemic Heart Disease LBBB Mitral Incompetence Mitral insufficiency Mitral valve prolapse Nocturia Patent Ductus Arteriosus PDA Polyuria Proteinuria pulmonary hypertension Pulmonary Stenosis ST Depression Symptoms of Acne Syncope Treatment for acne valvular heart disease Ventricular Septal Defect VSD Zits

Leave a Reply